Summary: The article shared a case of percutaneous puncture treatment for small nodules in the inferior lobe of right lung with Cryosurgical System. Professor Zou Yinghua of Peking University First Hospital commented on the case.
Basic information: Female, 61 years. The physical examination showed a small nodule lesion in the inferior lobe of the right lung, approximately 1.6 cm in diameter.
Chest CT findings: A nodule with heterogeneous density (SE203 IM170) in the anterior basal segment of the inferior lobe of the right lung adjacent to the diaphragm was observed, with acceptable boundary, local adjacent and pulling the pleura, ranging from approximately 1.6×1.6 cm in size, with cavitary lesions.
Presurgical examination: A refined echocardiographic examination showed abnormal findings in the left ventricular wall and outflow tract, which were considered possible as asymmetric obstructive hypertrophic cardiomyopathy. Subsequent coronary angiography and left ventricular pressure measurements showed a balanced type of coronary arteries, with no abnormalities in the left main trunk. A myocardial bridge was observed in the mid segment of the anterior descending branch, with systolic stenosis by 50%x1.5 cm. No significant stenosis was observed in the circumflex branch or the right coronary artery. Withdraw the TIG catheter and insert a Pigtail catheter into the left ventricle, the pressures measured upon withdrawal of the catheter were 211 mmHg in the left ventricular outflow tract and 111 mmHg in the aorta, which was considered as outflow tract obstruction.
Clinical diagnosis: Early-stage lung cancer in the right inferior lobe
MDT discussion: Due to poor cardiac function, the patient was deemed unsuitable for surgery. Therefore, co-ablation was performed on the pulmonary nodule lesions in the inferior lobe of the right lung with Cryosurgical System®.
Routine examination: The complete blood cell count as well as the liver and kidney function were normal.
Coagulation function: Normal.
Tumor indicators: Normal.
Preoperative Imaging Data
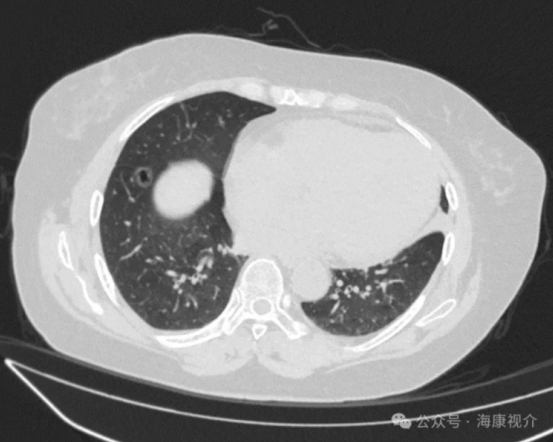
The chest CT scan on February 22, 2024, revealed a nodule with heterogeneous density (SE203 IM170) in the anterior basal segment of the inferior lobe of the right lung, adjacent to the diaphragm. It had well-defined borders and was locally adherent to and causing pleural retraction. The nodule measured approximately 1.6×1.6 cm and contained a cavity. These findings were suggestive of highly malignant lesions.
Cryosurgical System: The patient was positioned on their left side, with two ablation needles each measuring 2 mm in diameter arranged.
Characteristics of intraoperative ablation: The lesions were adjacent to the pleura and diaphragm. When using radiofrequency or microwave ablation, manual separation technology was required to separate the visceral pleura near the lesion from the parietal pleura. This separation was crucial to prevent pain from high-temperature stimulation and damage to the diaphragm. However, cryoablation did not require manual separation technology, and it caused no pain stimulation or damage to the diaphragm. Given the presence of a cavity in the lesion, normal saline was injected into the cavity before freezing. This facilitated the conduction of cold stimulation and ensured complete tumor eradication.
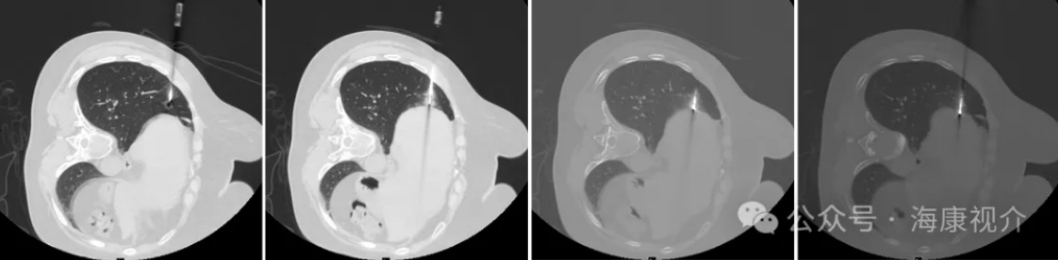
(Figure 1: Coaxial Sheath Puncture Lesion; Figure 2: Cavity Filled with Saline Injected Through Coaxial Sheath; Figure 3: Arrangement of 1 Cryosurgical System Needle at the Upper Pole of the Lesion; Figure 4: Arrangement of 1 Cryosurgical System Needle at the Lower Pole of the Lesion)
Cryosurgical System: 2 cycles
First cycle: freeze for 15 min and rewarm for 3 min;
Second cycle: freeze for 15 min and rewarm for 3 min.

CT Image After Freezing for 15 min
Ablation process - first cycle
(Freeze for 15 min + heat and rewarm for 3 min)
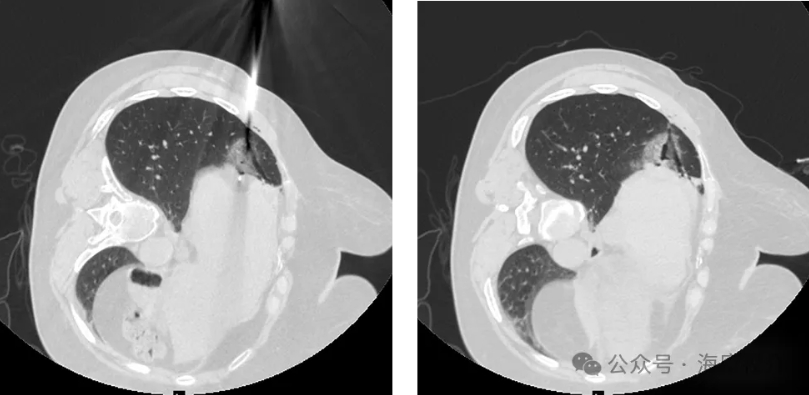
Left: CT Image After the Second Cycle of Freezing for 15 min; Right: CT Image After the Second Cycle of Rewarming and Needle Withdraw
Ablation process - second cycle
(Freeze for 15 min + heat and rewarm for 3 min, needle withdraw)
Postoperative Imaging Data
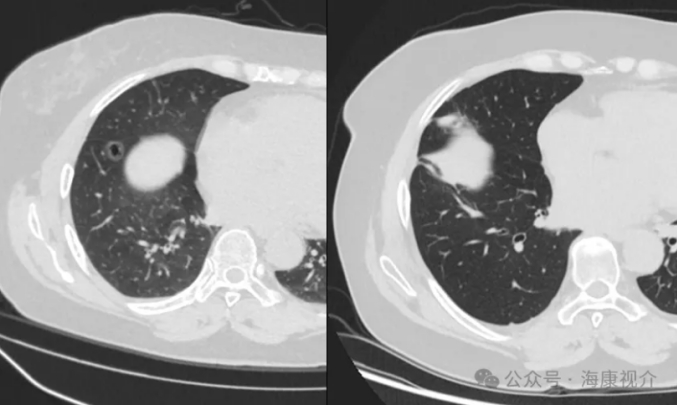
Left: Preoperative CT Image; Right: Postoperative CT Image After One Month
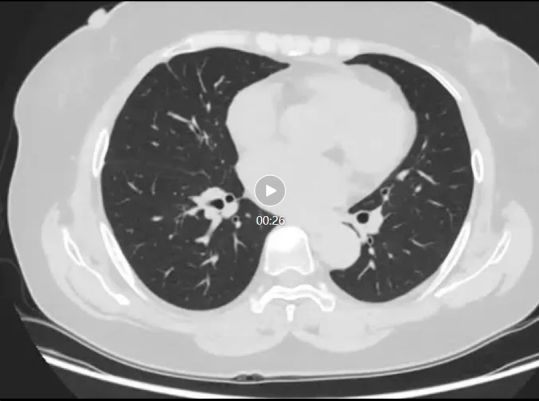
Postoperative CT Video After One Month
A 61-year-old female patient was diagnosed with early lung cancer based on a CT scan. However, surgery was deemed unsuitable due to poor cardiac function. Following a multidisciplinary team (MDT) discussion, coablation was performed with a 2-needle, 2-cycle regimen, which proved successful. The patient recovered well post-surgery and was discharged after 7 days.
One month later, a follow-up CT scan revealed complete disappearance of the original ground-glass nodule, with only streak shadows observed in the surgical area. The lung cancer was effectively cured."
Efficacy evaluation: Early lung cancer, characterized by ground-glass nodules, with low malignancy, can be cured with Cryosurgical System, which can achieve the same effects as surgeries. In the future, the ablation of ground-glass nodules was expected to be the mainstream solution.
Device use experience: For lesions near the pleura and diaphragm, the Cryosurgical System does not require manual separation technology. It causes no pain or damage to the diaphragm, ensuring safety and effectiveness. Local inflammation resulting from cryoablation is mild and typically resolves within one month. Efficacy is confirmed through follow-up examinations one month post-treatment.
Evaluation of the regimen: The lesion was located in the basal segment of the inferior lobe of the right lung, adjacent to the pleura and diaphragm. A CT scan revealed a typical malignant nodular lesion with central cavitation-like findings. Professor Hu's choose Cryosurgical System as the optimal treatment regimen. It not only achieved treatment outcomes comparable to surgical resection of lung segments but also mitigated risks such as parietal pleural pain and diaphragm damage associated with high-temperature stimulation from thermal ablation technologies. Furthermore, the procedure was pain-free throughout, significantly enhancing the patient's medical experience.
Professor Hu demonstrated extensive experience with the Cryosurgical System. When a cavity was identified within the lesion prior to surgery, injecting normal saline significantly enhanced the system's effectiveness in deactivating tumor cells. Overall, the case was characterized by a clear diagnosis, a well-considered treatment plan, precise surgical execution, and notable therapeutic outcomes, making it a valuable case for dissemination and learning.
Comment on Cryosurgical System: The Cryosurgical System, developed and produced in China as a high-end medical device, boasts advanced technology and user-friendly operation, yielding significant treatment benefits. In this case study, the system notably minimized intraoperative pain, facilitated quicker postoperative recovery, and enhanced overall patient comfort. Given these advantages, there is a strong recommendation for widespread adoption and promotion of the Cryosurgical System. Its positive impact on patient outcomes underscores its potential as a preferred option in medical practice.
Surgeon: Professor Hu Libao
Surgical team: Professor Hu Libao leads the Thoracic Surgery Department at Peking University People’s Hospital and serves as the Deputy Director of the Lung Cancer Center. He holds the position of Associate Chief Physician and specializes in various aspects of interventional treatment for chest diseases. His expertise includes percutaneous biopsy and ablation of chest tumors, preoperative puncture and positioning of small pulmonary nodules, transarterial chemoembolization for lung cancer and solid tumors, as well as interventional embolization treatment for conditions like hemoptysis and pulmonary arteriovenous malformation. Professor Hu's leadership and specialized skills contribute significantly to the advancement of thoracic surgery and interventional techniques at his institution.
Professor Zou Yinghua
Chief physician, professor, doctoral supervisor and former director of Interventional Vascular Surgery Department, Peking University First Hospital
Director of Oncology Minimally Invasive Intervention Department, Beijing GoBroad International Hospital, GoBroad Healthcare Group
Executive Director, Special Committee on Interventional Medicine of the National Health Commission Capacity Building and Continuing Education Center
Leader of the Special Ability Training Project on Oncology Minimally Invasive Intervention and Peripheral Vascular Intervention of the National Health Commission
Chairman of the Intelligent Vascular and Minimally Invasive Intervention Innovation Branch of the Chinese Medical Information and Big Data Association
Former vice president of Chinese College of Interventional Physicians of Chinese Medical Doctor Association
Deputy chairman of Bleeding Committee of the Chinese Research Hospital Association
Former chairman of Special Committee on Interventional Oncology of China Anti-cancer Association
Deputy chairman of Liver Cancer Expert Committee of China International Exchange and Promotion Association for Medical and Healthcare
Deputy leader of Haematology Group of Emergency Branch of Chinese Medical Association
Former chairman of Interventional Medicine Branch of Beijing Medical Association
Deputy chairman of Vascular Surgery Branch of Beijing Medical Association
 Hygea Medical Technology Co., Ltd.
Hygea Medical Technology Co., Ltd.